Case: A 25 yo F brought to your community emergency department after a motor vehicle crash where she was found ejected from the car. She initially had vital signs but lost them on route. EMS brings the patient to your community emergency department instead of the trauma hospital because it is the closest one. They are doing CPR on arrival.
What would you do?
a) Continue CPR as per ACLS protocol only pausing every 2 minutes for rhythm check
b) Continue CPR but pause for however long it takes to do any necessary procedures
Answer
B: Pause CPR for however long it takes to do the necessary life saving interventions.
Hey Doc, you are saying to PAUSE CPR when a person has NO PULSE? Isn’t that the OPPOSITE of what ACLS tells us to do?
YES, in blunt or penetrating trauma the rate of survival after cardiac arrest is quite poor. The mortality rate has been found to be as high as 96- 98%
CPR has NOT been shown to increase survival.
The causes of cardiac arrest in trauma are DIFFERENT than in a non-trauma case. In NON-traumatic cases, the most common cause of medical cardiac arrest is a CARDIAC cause. IE the heart CANNOT beat.
In cases of trauma, the causes of cardiac arrest are different – ie hypoxia, inadequate preload- hypovolemia, hemorrhage, obstructive shock- pericardial tamponade, hemo/pneumothorax, etc. So the heart CAN beat, but there is NO VOLUME or something is BLOCKING it. So doing CPR is futile because there is NOTHING to PUMP.
Ok, but can CPR be BAD?
In Trauma what actually HELPS is focusing on the reversible causes and actually treating them- Ie finger thoracostomy, intubation. Ie FIX the REVERISBLE Causes!
In a community hospital resources are often limited. There are often not enough nurses and physicians to run the code, and focusing primarily on CPR can distract from actual LIFESAVING interventions. IE if personnel are too focused on doing proper CPR, drawing up the epinephrine, etc, there may not be someone available to get the chest tube tray, intubation equipment, setting up MTP/ Rapid transfuser etc. Priority needs to be given to these lifesaving actions.
Also doing CPR while doing these procedures can increase risk of injury to the providers and decrease chance of success.
As per the European Resuscitation Council, “chest compressions take a lower priority than addressing the reversible causes. Chest compressions must not delay immediate treatment of reversible causes”
So if doing CPR makes you more comfortable, fine. Though do NOT delay other interventions because of CPR, and actually PAUSE CPR when you do the procedures (ie intubation, chest tubes etc), for faster/ greater success.
It is safe to PAUSE CPR for 3-5 minutes while addressing these other priorities.
What about epinephrine?
Once again interventions that are useful for medical cardiac arrest may NOT be useful during trauma. Epinephrine causes peripheral vasoconstriction, which can cause end organ damage and dysfunction. In certain studies they found that those who received epinephrine had higher rates of mortality and other studies found no improvement in survival rate.
Conclusion: Epinephrine has minimal benefit and could distract from useful solutions. Focus should be on the Lifesaving interventions
Ok Doc, So CPR is not useful, Epinephrine is NOT useful; so what DO we do in traumatic Cardiac Arrests?
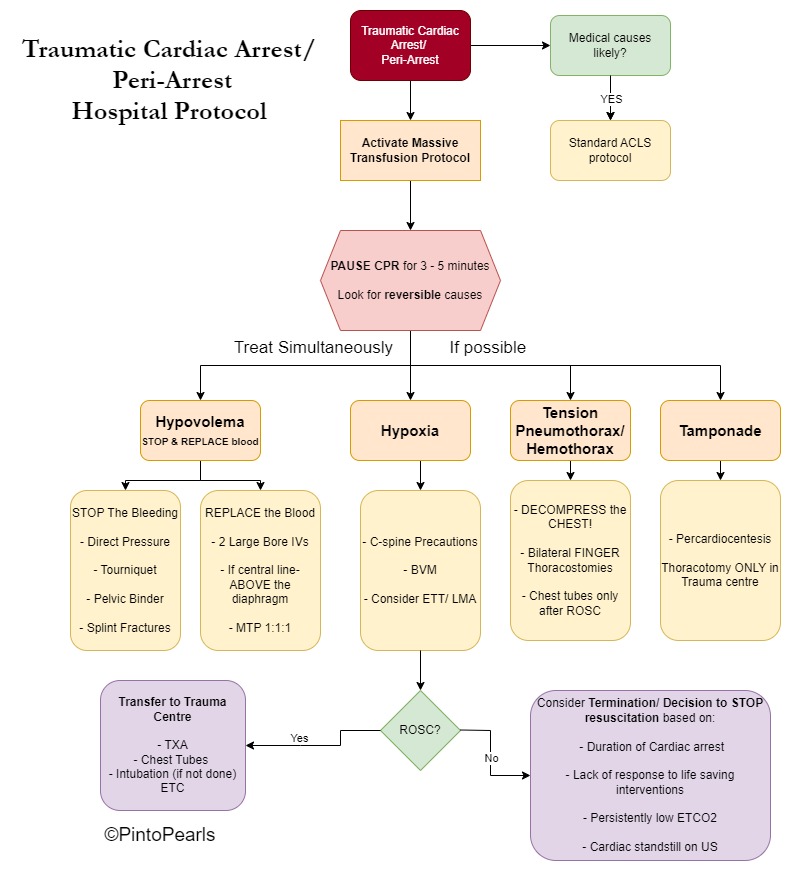
Great question! You should treat the REVERSIBLE Causes! These interventions should ideally be done SIMULTANEOUSLY. However, in resource limited environments they may need to be done sequentially. The main reversible causes are:
- Hypovolemia/ Hemorrhage
- Hypoxia,
- Tension pneumothorax/ Hemothorax,
- Tamponade
Also see the flow diagram at the end
| Cardiac Arrest Causes | Interventions |
| Hypovolemia / Hemorrhage | Control Hemorrhage/ Bleeding & Replace – STOP the blood from pouring out – Ie Pressure dressing, Tourniquet, Pelvic Binders, splint fractures etc. -Replace the Blood -> Blood Products, MTP o Central line ABOVE the Diaphragm! |
| Hypoxia | – BVM until you can Secure the Airway – Supraglottic Airway (LMA)/ Intubation |
| Tension Hemo/Pneumothorax | Decompress the Chest – Bilateral Finger Thoracostomies o IE you do NOT need to put a chest tube in. o Just decompress the area first w/ scalpel and Kelley. It is faster and more effective! o Come back later once the patient is stable to put in the chest tube |
| Tamponade | – Ultrasound to check for pericardial tamponade – Ultrasound guided pericardiocentesiso (+/- Thorocotomy -> ONLY if you have a trauma surgeon available) |
Note:
Please note that some trauma cases can be a mixed trauma/ medical cases– Ie an 80 year old in an isolated MVC with Cardiac arrest- Did the trauma/MVC cause the cardiac arrest, or did a medical cause (MI/ Bleed etc) cause the MVC. So it is important to consider medical causes even in trauma cases. If it is likely to be a primary medical cause you would treat as per ACLS protocol (Ie CPR, and Epi), though the interventions listed above will still be helpful.
The algorithm suggested above is referring to primarily TRAUMA Victims- ex the young pt with MVC, The pedestrian vs MVC, gunshot, stabbings etc.
Summary
- Make sure to consider/ rule out MEDICAL causes of cardiac arrest
- If the patient has a primary TRAUMATIC cause of cardiac arrest, then CPR and epinephrine are not likely to be helpful
- Focus should be on trying to address: Hypovolemia/ Hemorrhage, Hypoxia, Tension Hemo/pneumothorax, Tamponade
- Interventions include: Controlling the bleed, replacing the blood, BVM/ Intubation, Bilateral finger thoracostomies, pericardiocentesis
- MAYBE thoracotomy- though unlikely in a community hospital
- STOP CPR when doing the procedures.
- Remember – survival rate is generally poor for traumatic cardiac arrests, so despite your best attempts, the patient may not survive
References/ Further Reading
- Bledsoe, B. E., & Salomone, J. P. (2023). Traumatic cardiac arrest (TCA): Maybe we could do better? Journal of Emergency Medical Services
- Costain, N., & Suttie, R. (2018). Management controversies in traumatic cardiac arrest. EMOttawa Blog
- Crewdson, K., & Lockey, D. (n.d.). Mortality in traumatic cardiac arrest. Resuscitation. Retrieved November 25, 2023
- Truhlář, A., Deakin, C. D., Soar, J., et al. (2021). European resuscitation council guidelines for resuscitation 2021: Section 4. Cardiac arrest in special circumstances. European Resuscitation Council Guidelines
- The Royal Children’s Hospital. (n.d.). RCH trauma guideline – Management of traumatic pneumothorax and haemothorax
- Vianen, N. J., et al. (2022). Prehospital traumatic cardiac arrest: A systematic review and meta-analysis. European Journal of Trauma and Emergency Surgery: Official Publication of the European Trauma Society. U.S. National Library of Medicine
- Konesky, K. L., & Guo, W. A. (n.d.). Revisiting traumatic cardiac arrest: Should CPR be initiated? European Journal of Trauma and Emergency Surgery: Official Publication of the European Trauma Society. U.S. National Library of Medicine