
Clinical Scenario: A 38-year-old male presents to the emergency department after experiencing an electrical shock while working on a household toaster with un-gloved hands. The patient describes the shock as more severe than any previous experience but currently denies any symptoms. Initial examination reveals stable vital signs, normal neurological and cardiovascular and physical assessments and EKG. What is your plan for this patient?
- Discharge the patient with appropriate follow-up instructions
- Initiate fluid resuscitation and admit for observation
- Obtain a troponin level and continuous cardiac monitoring for 6-8 hours
- Perform a CT scan of the head and spine
…
Answer:
A: Discharge the patient!
Wait Doc, did you say DISCHARGE? But we did not do any blood work or a troponin!
Yes, like with most of emergency medicine, your HISTORY and CLINICAL EXAM are the most important when determining how to manage a patient.
IF the patient has a benign history, normal physical exam and normal EKG then blood work doesn’t add much to the management of the patient.
Ok, then so what are the some important questions to ask when evaluating an electrical injury?
In addition to your regular questions the following are important to determine in an electrical injury,
- What was the voltage of the device – < 600V or >600V?
- Prolonged Exposure or not
- Degree of “wetness”
- AC or DC current
- Any Symptoms currently
- Any Burns
- What was the voltage of the device – < 600V or >600V?
-
- Why?
- You want to know if it is a High Voltage (>1000V) or Lowvoltage (< 600V)
- Note- Some resources use 600 V as the threshold for high voltage, so 600V – 1000V use clinical discretion as to the management
- Low voltage injuries tend to have benign outcomes. See Table 1
- You want to know if it is a High Voltage (>1000V) or Lowvoltage (< 600V)
- Many may not know the Voltage so rule of thumb
- Low Voltage – Most Standard Household devices are LESS than 250V
- Example – Toaster, Electrical outlet, Television, Oven, Dryer etc
- High voltage- Construction Sites, Power lines, subway rails etc – have HIGH index of suspicion
- Low Voltage – Most Standard Household devices are LESS than 250V
- Why?
- Prolonged Exposure or not
- Ie were they holding the device for a prolonged time
- Why? This Increases degree of injury
- Degree of “wetness”
- Some Low voltage injuries may be more serious because of a wet environment
- Decreases the resistance and increases the degree of damage
- Ex a live electrical device in a bathtub
- Some Low voltage injuries may be more serious because of a wet environment
- AC or DC current
- AC (alternating current) – can cause prolonged contraction of muscle, (preventing release of object)causing prolonged exposure
- Note- typically harder to know immediately, and doesn’t affect your immediate management
- AC (alternating current) – can cause prolonged contraction of muscle, (preventing release of object)causing prolonged exposure
- Any Symptoms currently
- Ex CHEST PAIN, ear loss, vision changes etc
- Any Burns
- Note burns may be deeper than the superficial manifestation
- Though Low voltage burns tend to only have superficial injries
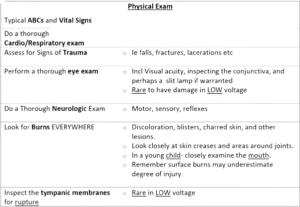
OK doc, So I have asked these questions, but What are some key things on physical exam that I should be paying attention to?
- Typically low voltage exposure have very minimal injuries
- On ALL patients evaluate the following:
Ok, I’ve taken the History and Done the Physical, is there any TEST that I should do?
- An ECG! This should be done on EVERYONE!
- There are reports of myocardial infarction, arrhythmia, and other ECG abnormalities after both low- and high-voltage exposure.
What am I MOST LIKELY to see on ECG?
- Usually NOTHING or Sinus Tachycardia
- May see (Though uncommon if <120V)
- 1st and 2nd degree AV blocks
- Atrial fibrillation
- Premature ventricular complexes, (PVCs)
- Note- the above are typically seen within the first couple of hours and tend to self-resolve
Any SERIOUS ECG Findings
Yes, but they are MUCH Less Common but important to know
- Ventricular fibrillation – Most common fatal dysrhythmia
- Typically Occurs RIGHT AWAY
- Treat as normal ACS- Shock!
- Asystole – for High voltage currents
- Rare, immediate
- Myocardial infarction – RARE
Wait Doc, what about the TROPONIN?
- A troponin is NOT useful if the patient has a:
- LOW voltage exposure (<600V),
- ASYMPTOMATIC – ie NO chest pain, no burns,
- NO shortness of breath etc and
- NORMAL ECG-
- A troponin is only helpful if we are suspecting an MI or cardiac contusion – both of which are quite rare
What about a CK? Blood work ETC?
- In low voltage injuries the incidence of rhabdomyolysis and compartment syndrome are rare. Discharge instructions should be given so that patients return if there are signs of it, though they are uncommon
Ok doc, What now? Who do we discharge? Who do we ADMIT?
See below for the algorithm:
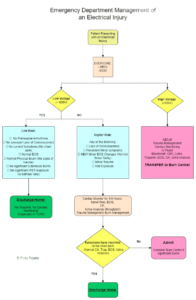
You can Discharge the patient if:
- Low voltage (<600V)
- Asymptomatic- no chest pain, no current symptoms
- No reported loss of consciousness
- Normal physical exam
- Normal ECG
- NOTE: NO Cardiac Monitoring, NO Bloodwork/ Troponin Needed
Observation in ED with Cardiac Monitoring if
- Low Voltage Exposure (<600V) BUT Higher Risk
- Skin wet during injury
- May have had tetany/ significant muscle contractions
- Symptomatic- Ex chest pain
- High risk for cardiac complications- significant cardiovascular history etc
- Loss of consciousness
- Mild cutaneous burns
- Minor Abnormalities on ECG
- Note- Can discharge these patients after 4-6 hours of cardiac monitoring if:
- No more symptoms
- Normal ECG
- (Or has normalized after monitoring)
- Normal blood work- troponins, CK, Urine myoglobin
- Normal cardiac monitoring
Admit the patient if
- High Voltage
- See Next blog post for full management!!
- Deep Skin and Local Soft tissue burn
- RARE – but happens if patient was unable to “let go” of current
- May have deeper burns than seen externally
- TRANSFER to BURN center for evaluation – may need more extensive repair
- RARE – but happens if patient was unable to “let go” of current
- Major ECG abnormalities
- Failed above discharge criteria
- Consider Transfer to Burn Unit
Any Discharge instructions?
- YES! Discharge instructions are VERY IMPORTANT!
- Advise patients that
- Delayed neurologic symptoms may occur, even psychological- difficulty concentrating etc
- They should return if signs of chest pain, palpitations, syncope, and compartment syndrome – increased pain/ swelling in a particular limb.
Any Special Populations we should be paying attention to?
- Yes!
- Pediatrics patients and Pregnant women
- But stay tuned to the next blog for management of these patients!
So Back to the Case:
The patient was working with a toaster- ie Low volatage, no symptoms, normal physical exam, and normal EKG,
So DISCHARGE would be best in this scenario
Summary
- Electrical injuries have a full spectrum of presentation
- Important questions to ask are:
- What was the voltage of the device – < 600V or >600V? , was there a Prolonged Exposure or not, what was the Degree of “wetness”, what was the current, Any Symptoms currently, Any Burns
- Important to do a full physical exam
- An ECG is required on EVERYONE
- Can safely discharge the patient with NO bloodwork or ECG if:
- Low voltage (<600V)
- Asymptomatic- no chest pain, no current symptoms
- No reported loss of consciousness
- Normal physical exam
- Normal ECG
- For management of High Voltage patients or Special populations see: The NEXT BLOG!


1 Comment