
Hey Doc, His Blood Pressure is 200/ 110. What do we do?
Today we are going to talk about Blood Pressure! When do we need to worry and send the patient to the Emergency Room and when can we just let it be?
Let’s dive into Some Cases!
Case:
Case 1– Patient comes to the ED sent by the GP with a BP of 200/110 and a history of hypertension. No symptoms. What do you do?
Case 2- Patient is coming in with headaches/ migraines and a history of headaches & Migraines. Blood Pressure is 180/105. What do you do?
Case 3- Patient is coming in a laceration to his hand. Blood pressure is 200/100. No known history of hypertension, but no symptoms. What do you do?
Case 4- Patient is coming in with new onset headache, blood pressure is 180/105. No known history of hypertension. What do you do?
Case 5- Patient is brought in by husband because she is acting confused, no history of confusion. No fevers, or any other symptoms. Blood pressure is 185/90. No known history of hypertension. What do you do?
Answer
Hypertension is a common presenting complaint in the emergency and depending on the physician and nurse assessing can have a wide range in workup from nothing, to everything. When does a high blood pressure need to be treated? When can it be left alone?
Important Questions to Answer:
Are they Pregnant?
-
- Pregnant patients are excluded from this management approach, since pre-eclampsia is a risk and should be managed differently
Is there evidence of END ORGAN DAMAGE:
- Need to assess the 3 areas that could be affected
-
-
- 1) The Brain
- Sudden onset of severe headache -> Subarachnoid Hemorrhage
- Signs of stroke or neurologic conditions
- Focal Neurologic Deficit
- Vision loss
- Altered mental status/ Confusion
- Seizure
- 2) The Heart / Lungs
- Chest Pain/ Epigastric pain- concerning for acute myocardial ischemia or acute aortic dissection
- Respiratory distress, hypoxia, volume overload, pitting edema -> Signs of Heart Failure
- 3) The Kidneys
- Oliguria, NOT making urine, pitting edema,
- Oliguria, NOT making urine, pitting edema,
- 1) The Brain
-
- Physical Exam should include
- Full Neurologic Exam, Full cardiovascular Exam, Full Respiratory Exam.
- NOTE: Patients with asymptomatic hypertension may have mild symptoms such as mild headache or lightheadedness, but this does not necessarily indicate need to search for end-organ damage
If NO evidence of end organ damage, this is NOT a Hypertensive Emergency.
-
It could be considered a “Hypertensive Urgency” (this classification/term is no longer used) – ie severe BP elevation in otherwise stable patients without acute or impending change in target organ damage or dysfunction. (ACC 2017)
If NO hypertensive emergency, do NOT aggressively lower blood pressure
- “There is no indication for referral to the emergency department, immediate reduction in BP in the emergency department, or hospitalization for such patients.”
- 2017 American Heart Association and American College of Cardiology Guidelines
- 2017 American Heart Association and American College of Cardiology Guidelines
- The patient does NOT need acute blood pressure lowering in the ED, and does NOT need IV Medications
- American College of Emergency Physicians 2013 Guidelines
- American College of Emergency Physicians 2013 Guidelines
- EVEN if BP > 200, patient does NOT need IV medications OR Resus / Acute bed, UNLESS signs of End organ damage
- Just start on PO meds- ex Captopril (if you need ACUTE lowering of meds)
- Just start on PO meds- ex Captopril (if you need ACUTE lowering of meds)
- Note- Rapidly lowering blood pressure could theoretically CAUSE a stroke due to hypo-perfusion of the brain, especially in patients with chronically high blood pressure
- So- MAX drop of 20% in blood
But Doc, What about Blood work?
ACEP 2013 Guidelines
-
-
Routine screening for acute target organ injury (e.g. creatinine, UA, ECG) is NOT required
- In select patient populations, screening of creatinine may identify injury that affects disposition
- IF Diastolic < 120 -> No ED Work up needed
- If Systolic > 210 BPM OR Diastolic > 120 – 130
- Consider: CBC, Chemistry (Creatinine)
- IF Normal, Outpatient treatment sufficient
- Consider: CBC, Chemistry (Creatinine)
-
-
- “No other diagnostic screening tests (e.g. UA, ECG) appear to be useful”
So then what do we do? Anything?
- If prior history of high blood pressure -> restart/ adjust medications
- If NO history of high blood pressure, can consider starting on an ORAL antihypertensive
- Do NOT need to see significant drop in blood pressure before discharging home
- ** Arrange CLOSE Follow up!
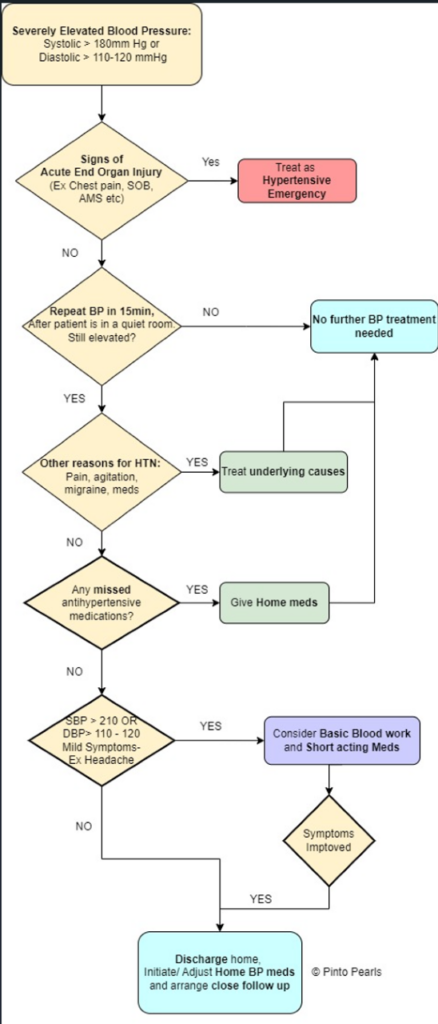
- **SEE FLOW DIAGRAM Below ( Attached)
Clinical Pathway for Elevated Blood Pressure
Commonly used Oral Antihypertensive Medications in ACUTE setting
| Agent | Class | Onset of Action | Duration of Action | Dosing | Adverse Effects |
| Captopril ** (preferred) | ACE-I | 5 – 15 minutes | 2 – 6 hr | 25mg PO/SL Range: 6.25 – 50mg PO (max) | ACE-I side effects: Hyperkalemia, angioedema, etc |
| Labetalol | a1- selective, B-Blocker | 2 hrs | 4 hr | 200mg PO, followed by 200mg PO Q1-2hrs until desired effect | Hypotension, dizziness, headache, nausea |
| Amlodipine | Calcium channel blocker | 4-6 hrs | 24 – 72 hrs | 5 – 10 mg PO | peripheral edema, dizziness, palpitations, and flushing |
Often adjusting or initiating LONGER term antihypertensive is preferred to ACUTELY lowering BP
Note- Amlodipine takes LONG to work, so may not see effect until ~ 4hrs later
Case Resolutions
Case 1- Patient comes to the ED sent by the GP with a BP of 200/110 and a history of hypertension. No symptoms. What do you do?
- Answer: Follow diagram. Treat as asymptomatic Hypertension. Consider starting new oral hypertensives as outpatient and arrange close follow up.
Case 2- Patient is coming in with headaches/ migraines. History of headaches & Migraines. Blood Pressure is 180/105. What do you do?
- Answer: Treat the migraine first, recheck the blood pressure after. If the headache resolves and blood pressure improves, can conclude that headache is secondary to pain/ migraines. If not, further workup MAY be necessary
Case 3- Patient is coming in with a laceration to his hand. Blood pressure is 200/100. No known history of hypertension, but no symptoms. What do you do?
- Answer: Arrange close follow up. Can consider starting low dose of new oral hypertensives.
Case 4- Patient is coming in with new onset headache, blood pressure is 180/105. No known history of hypertension. What do you do?
- Answer: Showing mild symptoms. Do initial workup and slowly decrease the blood pressure. Reassess to see if any signs of symptom improvement.
Case 5– Patient is brought in by husband because she is acting confused, no history of confusion. No fevers, or any other symptoms. Blood pressure is 185/90. No known history of hypertension. What do you do?
- Answer: Treat as hypertensive emergency! Patient Showing signs of end organ dysfunction!

